Prostate Cancer Treatment Specialist

Do you have blood in your urine or burning pain while urinating? These symptoms could indicate the presence of many other diseases or disorders, but could be prostate cancer. If you have similar symptoms, or have been diagnosed with prostate cancer, you need someone who has extensive experience in successfully treating urological diseases. Prostate cancer treatment specialist, Dr. Mark Allen provides diagnosis and both surgical and nonsurgical treatment options for patients in Plano who are suffering from symptoms of prostate cancer. Contact Dr. Allen’s team today!
An Overview of Prostate Cancer Treatment
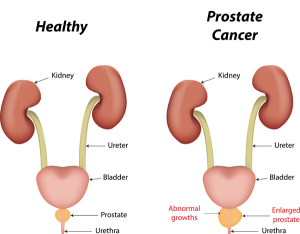
Prostate cancer is defined as cancer that begins in the prostate gland. Prostate cancer can strike any male for a number of varying reasons. Men who have had prostate problems in the past, who have a family history of the disease and those who have poor dietary habits and who abuse alcohol may be at a higher risk. The symptoms of prostate cancer appear differently from one victim to another. But symptoms that are most alarming, and may directly relate to the onset of prostate cancer, is blood found in the urine and a burning pain while urinating. If these symptoms occur in Plano, Frisco and Dallas, Texas area men, Dr. Mark Allen, board certified urologist, is available to help determine if a prostatectomy is the ideal prostate cancer treatment.
Prostate Cancer Symptoms
If prostate cancer is caught at its earliest stages, most men will not experience any symptoms. However, some men will experience symptoms that might indicate the presence of prostate cancer, including:
- A need to urinate frequently, especially at night;
- Difficulty starting urination or holding back urine;
- Weak or interrupted flow of urine;
- Painful or burning urination;
- Difficulty in having an erection;
- Painful ejaculation;
- Blood in urine or semen; or
- Frequent pain or stiffness in the lower back, hips, or upper thighs.
These symptoms can also indicate the presence of many other diseases or disorders, such as enlarged prostate (BPH) or prostatitis. Therefore, men who experience any of these symptoms will undergo a thorough work-up to determine the underlying cause of the symptoms.
Prostate Cancer Diagnosis
If the above symptoms exist or suspicious results are found through screening tests for early detection such as the prostate-specific antigen (PSA) blood test and or digital rectal exam (DRE), Dr. Allen will request that you schedule a prostate biopsy to find out if the disease is present. A biopsy is a 15 minute procedure a performed in the North Dallas Urology office. A sample of your body tissue is removed and then looked at under a microscope. A core needle biopsy is the main method used to diagnose prostate cancer. Your tissue sample will be sent to a lab for analysis to determine if there are any cancer cells present.
Positive Prostate Cancer Biopsy Results
Once cancer cells are found in your tissue sample, the pathologist will then grade your cancer according to the Gleason system. This system assigns a Gleason grade, using numbers from 1 to 5 based on how much the cells in the cancerous tissue look like normal prostate tissue.
- If the cancerous tissue looks much like normal prostate tissue, a grade of 1 is assigned.
- If the cancer lacks these normal features and its cells seem to be spread haphazardly through the prostate, it is called a grade 5 tumor.
- Grades 2 through 4 have features in between these extremes.
Because prostate cancers often have areas with different grades, a grade is assigned to the 2 areas that make up most of the cancer. These 2 grades are added together to yield the Gleason score (also called the Gleason sum) between 2 and 10.
- Cancers with Gleason scores of 2 to 4 are sometimes called well-differentiated or low-grade.
- Cancers with Gleason scores of 5 to 7 may be called moderately-differentiated or intermediate-grade.
- Cancers with Gleason scores of 8 to 10 may be called poorly-differentiated or high-grade.
The higher your Gleason score, the more likely it is that your cancer will grow and spread quickly.
In addition to the grade of the cancer, the pathologists report may also contain other pieces of information that may give a better idea of the scope of the cancer including:
- the number of biopsy core samples that contain cancer (for example, “7 out of 12”)
- the percentage of cancer in each of the cores
- whether the cancer is on one side (left or right) of the prostate or both sides (bilateral)
False Negatives and Suspicious Results
Even with many samples, biopsies can still sometimes miss a cancer if none of the biopsy needles pass through it. This is known as a “false negative” result. If your doctor still strongly suspects prostate cancer due to a very high PSA level or other symptoms, a repeat biopsy may be recommended.
There are also cases where the pathologist looks at the prostate cells under the microscope and they do not look cancerous, but they’re not quite normal, either. These results are typically reported as suspicious. They generally fall into 2 categories: prostatic intraepithelial neoplasia (PIN) or atypical small acinar proliferation (ASAP).
In PIN, there are changes in how the prostate cells look under the microscope, but the abnormal cells don’t look like they’ve grown into other parts of the prostate (like cancer cells would). PIN is usually divided into low-grade and-high grade. Many men begin to develop low-grade PIN at an early age but do not necessarily develop prostate cancer.
If high-grade PIN is found on a biopsy, there is about a 20% chance that cancer may already be present somewhere else in the prostate gland. In this situation, doctors often watch men with high-grade PIN carefully and may advise a repeat prostate biopsy, especially if the original biopsy did not take samples from all parts of the prostate.
Another finding sometimes reported on a prostate biopsy is atypical small acinar proliferation (ASAP), which is sometimes just called atypia. In ASAP, the cells look like they might be cancerous when viewed under the microscope, but there are too few of them to be sure. If ASAP is found, there’s about a 40% to 50% chance that cancer is also present in the prostate, which is why many doctors recommend getting a repeat biopsy within a few months.
Prostate Cancer Treatment Considerations
Once your prostate cancer has been diagnosed, graded, and staged, you need to consult with your doctor and family to determine which prostate cancer treatment option is the best fit with your specific diagnosis, age and lifestyle. It is important for you to take the time to absorb the information and seriously consider all of your options before making a final decision on which treatment is best for you.
The treatment you choose for prostate cancer should take into account:
- your age and expected life span
- any other serious health conditions you may have
- the stage and grade of your cancer
- your feelings (and your doctor’s opinion) about the need to treat the cancer
- the likelihood that each type of treatment will cure your cancer or provide a benefit
- your feelings about the side effects common with each treatment
Prostatectomy and Other Prostate Cancer Treatments
There are several different types of prostate cancer treatment available for patients. Some treatments are widely used and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to newly diagnosed patients.
Four types of standard prostate cancer treatments are used:
Watchful waiting – closely monitoring a patient’s condition without giving any treatment until symptoms appear or change. This is usually used in older men with other medical problems and early-stage disease.
Surgery – patients in good health are usually offered surgery as treatment for prostate cancer. The potential side-effects of surgery are impotence and leakage of urine from the bladder or stool from the rectum. In some cases, doctors can use a technique known as nerve-sparing surgery. This type of surgery may save the nerves that control erection. Unfortunately, men with large tumors or tumors that are very close to the nerves may not be able to have this surgery. The following types of surgery are used to treat prostate cancer:
- Pelvic lymphadenectomy: Lymph nodes are removed surgically in the pelvis. A pathologist views the tissue under a microscope to look for cancer cells. If the lymph nodes contain cancer, the doctor will not remove the prostate and may recommend other treatment.
- Radical prostatectomy: A surgical procedure to remove the prostate, surrounding tissue, and seminal vesicles. There are various types of radical prostatectomy:
- Traditional open procedure: surgeon uses an 8-10 inch incision to access the prostate. This approach often results in substantial blood loss and long, uncomfortable recovery.
- Conventional laparoscopy: a specialized surgical camera and rigid instruments to access and remove the prostate using a series of small incisions. Conventional laparoscopy relies on rigid instruments and standard 2D video, technical limitations that can be challenging for the surgeon. Because of these drawbacks, conventional laparoscopy doesn’t lend itself well to complex procedures like prostatectomy. Therefore, very few urologists use this approach for prostatectomy.
- da Vinci prostatectomy is a robotic-assisted radical prostatectomy performed in a minimally invasive approach. Surgeons have demonstrated (and widely published) results with da Vinci prostatectomy that offer excellent rates of cancer control while speeding the return of urinary continence and sexual function.
- Transurethral resection of the prostate (TURP): A surgical procedure to remove tissue from the prostate using a resectoscope (a thin, lighted tube with a cutting tool) inserted through the urethra. This procedure is sometimes done to relieve symptoms caused by a tumor before other cancer treatment is given. Transurethral resection of the prostate may also be done in men who cannot have a radical prostatectomy because of age or illness.
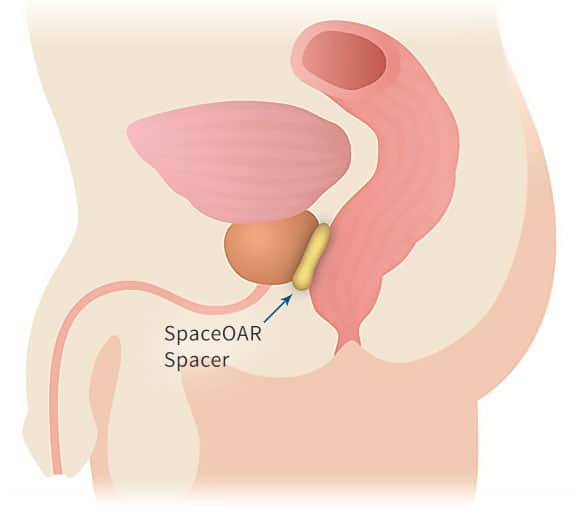
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy. External radiation therapy which uses a machine outside the body to send radiation toward the cancer. Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer. The way the radiation therapy is given depends on the type and stage of the cancer being treated. The side effects of radiation therapy can be impotence, urinary problems and accidental damage to the rectum. (Learn more about SpaceOAR Hydrogel for rectum-sparing prostate radiation therapy.)
Hormone therapy (androgen deprivation therapy) may be used in conjunction with other treatments or alone as a primary treatment. Hormone therapy may act to halt or slow the growth of prostate cancer, and it is often used in men with advanced disease. A variety of hormonal drugs can produce a medical castration by cutting off supplies of male hormones. Female hormones (estrogens) block the release and activity of testosterone. Antiandrogens block the activity of any androgens circulating in the blood. Still another type of hormone, taken as periodic injections, prevents the brain from signaling the testicles to produce androgens. Hormone Therapy has the potential to cause a number of side effects such as impotence, hot flashes and weakened bones.
Cryosurgery: (cryotherapy) uses liquid nitrogen to freeze and kill prostate cancer cells. Guided by ultrasound, the doctor places needles in pre-selected locations in the prostate gland. The needle tracks are dilated for the thin metal cryo probes to be inserted through the skin of the perineum into the prostate. Liquid nitrogen in the cryo probes forms an ice ball that freezes the prostate cancer cells; as the cells thaw, they rupture. The procedure takes about two hours, requires anesthesia (either general or spinal), and requires one or two days in the hospital. During cryosurgery, a warming catheter inserted through the penis protects the urethra, and incontinence is seldom a problem. However, the overlying nerve bundles usually freeze, so most men become impotent. The appearance of prostate tissue in ultrasound images changes when it is frozen. To be sure enough prostate tissue is destroyed without too much damage to nearby tissues, the surgeon carefully watches these images during the procedure. But compared with surgery or radiation therapy, doctors know far less about the long-term effectiveness of cryosurgery. Current techniques using ultrasound guidance and precise temperature monitoring have only been available for a few years. Outcomes of long-term (10- to 15-year) follow-up must still be collected and analyzed. For this reason, most doctors do not include cryosurgery among the options they routinely consider for initial treatment of prostate cancer.
For additional resources on prostate cancer treatment options, including a prostatectomy, please contact the practice of Dr. Mark Allen, urologist serving the communities of Plano, Frisco and Dallas, Texas.